NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) with NCCN Evidence Blocks™
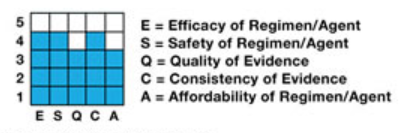
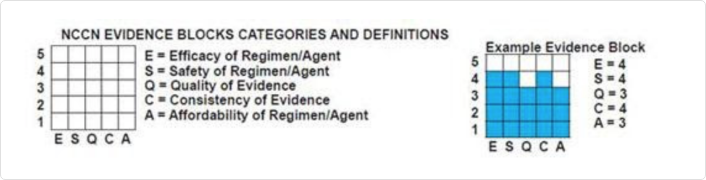
NCCN Evidence Blocks™ are intended as a visual representation of five key measures that provide important information about specific systemic therapy recommendations contained within the NCCN Guidelines.
- Efficacy of Regimen/Agent
- Safety of Regimen/Agent
- Quality of Evidence
- Consistency of Evidence
- Affordability of Regimen/Agent
NCCN EVIDENCE BLOCKS CATEGORIES AND DEFINITIONS
© National Comprehensive Cancer Network®
The goal is to provide the health care provider and the patient information to make informed choices when selecting systemic therapies based upon measures related to treatment, supporting data, and cost. These measures may be used to understand the clinical and scientific rationale for specific recommendations and estimates of the economic impact of the recommendations. They may also be used to educate providers and patients, and as a starting point for shared decision-making considering the patient's value system.
With the availability of a wide range of evidence-based therapies, clinicians and patients must choose the treatment that is most appropriate considering what matters most to the patient. Implicit in the evaluation of each treatment is the efficacy, quality, quantity, and consistency of the evidence supporting the recommendation as well as and expected associated toxicities. The NCCN Evidence Blocks™ make the panels' assessments of each of these parameters transparent to the users of the NCCN Guidelines.
The NCCN Evidence Blocks™ are subject to certain U.S. and foreign patents. Each approved use of the design of the NCCN Evidence Blocks™ requires the written approval of NCCN. Visit www.nccn.org/patents for current list of applicable patents.
To develop the NCCN Evidence Blocks™, NCCN Panel members score each measure using a standardized scale from "1" to "5" with "1" being the least favorable and "5" the most favorable. For efficacy and safety, panel members use both their knowledge of the published data—often developed in highly selected patients—and their clinical experience with the treatments in the real-world patient population. Quality and consistency of the data are rated using the panel members’ knowledge of the data supporting the treatment. Affordability is rated using the panel members’ knowledge of the overall cost of the regimen.
Resulting data are analyzed and final scores based on all responding panel members, rounding to the closest whole number. These scores are then used to build the 5 x 5 table that constitutes the NCCN Evidence Block™ for the intervention. Each column in the Evidence Block corresponds to an outcome characteristic. From left to right the outcome characteristics are efficacy (E), safety (S), quality and quantity of evidence (Q), consistency of evidence (C) and affordability (A). The rows of the block are shaded in from bottom to top representing the corresponding score for each measure.
The use of a graphical representation of the measures through NCCN Evidence Blocks™ allows for the efficient scanning and interpretation of multiple therapy options in a very efficient manner. When the NCCN Evidence Blocks™ are placed on the NCCN Guidelines algorithm, a user can quickly scan a group of potentially appropriate interventions and make treatment recommendations based on what is most important to the patient. Some patients will want an emerging therapy even with limited data; others will be most concerned about the expected side effects of the treatment indicated in the safety column. Still others may be very sensitive to cost. By considering the attributes of the range of possible therapies, the health care provider and the patient can discuss the benefits and drawbacks of each option and come to a decision most acceptable to the individual.
Panel members used the following criteria to score the measures.
[E] The Efficacy measure is the extent to which an intervention is helpful in prolonging life, arresting disease progression, or reducing symptoms of a medical condition. The scale used to measure efficacy is:
- 5 (Highly effective): Cure likely and often provides long-term survival advantage
- 4 (Very effective): Cure unlikely but sometimes provides long-term survival advantage
- 3 (Moderately effective): Modest impact on survival, but often provides control of disease
- 2 (Minimally effective): No, or unknown impact on survival, but sometimes provides control of disease
- 1 (Palliative only): Provides symptomatic benefit only
[S] Safety refers to the assessment of the relative likelihood of side effects from an intervention with fewer side effects being scored highly. The scale used to measure safety is:
- 5 (Usually no meaningful toxicity): Uncommon or minimal toxicities; no interference with activities of daily living (ADLs)
- 4 (Occasionally toxic): Rare significant toxicities or low-grade toxicities only; little interference with ADLs
- 3 (Mildly toxic): Mild toxicity that interferes with ADLs
- 2 (Moderately toxic): Significant toxicities often occur but life threatening/fatal toxicity is uncommon; interference with ADLs is frequent
- 1 (Highly toxic): Significant toxicities or life threatening/fatal toxicity occurs often; interference with ADLs is usual and severe
Note: For significant chronic or long-term toxicities, score decreased by 1
[Q] Quality and quantity of evidence refers to the number and types of clinical trials relevant to a particular intervention. To determine a score, panel members may weigh the depth of the evidence, i.e., the numbers of trials that address this issue and their design. The scale used to measure quality of evidence is:
- 5 (High quality): Multiple well-designed randomized trials and/or meta-analyses
- 4 (Good quality): One or more well-designed randomized trials
- 3 (Average quality): Low quality randomized trial(s) or well-designed non-randomized trial(s)
- 2 (Low quality): Case reports or extensive clinical experience
- 1 (Poor quality): Little or no evidence
[C] Consistency of evidence refers to the degree to which the clinical trials addressing an intervention have consistent results. The scale used to measure consistency of evidence is:
- 5 (Highly consistent): Multiple trials with similar outcomes
- 4 (Mainly consistent): Multiple trials with some variability in outcome
- 3 (May be consistent): Few trials or only trials with few patients, whether randomized or not, with some variability in outcome
- 2 (Inconsistent): Meaningful differences in direction of outcome between quality trials
- 1 (Anecdotal evidence only): Evidence in humans based upon anecdotal experience
[A] Affordability refers to the overall cost of an intervention including drug cost, required supportive care, infusions, toxicity monitoring, management of toxicity, probability of care being delivered in the hospital, etc. with less expensive interventions being rated more highly than more expensive ones. The scale used to measure affordability is:
- 5 Very inexpensive
- 4 Inexpensive
- 3 Moderately expensive
- 2 Expensive
- 1 Very expensive
Q. What are NCCN Evidence Blocks™?
NCCN Evidence Blocks™ are a visual representation of five key components of value that provide important information about specific recommendations contained within the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®). These five components are: efficacy, safety, quality and quantity of evidence, consistency of evidence, and affordability.
Q. Who are the intended users of NCCN Evidence Blocks™?
NCCN Evidence Blocks™ are intended for all users of NCCN Guidelines®, including providers and patients, as well as other stakeholders involved in the treatment decision-making process, as a means to initiate a discussion of value between a provider and patient. Together, the five measures–efficacy, safety, quality and quantity–of evidence, consistency of evidence, and affordability provide the individual information to make their own assessments of value.
Q. How are the criteria in NCCN Evidence Blocks™ scored?
To develop NCCN Evidence Blocks™, NCCN Guidelines panel members score each measure using a standardized scale from "1" to "5", with "1" being the least favorable and "5" being the most favorable.
For efficacy and safety, panel members use both their knowledge of the published data cited within the NCCN Guidelines—often developed in highly selected patients—and their clinical experience with treatment in the more diverse real-world patient population.
Quality and consistency of data are rated using evidence cited within the Guidelines and the panel members' knowledge of the data supporting the treatment.
Affordability is rated using and the panel members' knowledge of overall cost of the regimen, including cost of drug, administration, required supportive care, identification and management of toxicity and probability of hospitalization.
Q. How do you read an NCCN Evidence Block™?
Final scores from the NCCN Guidelines panel members' analysis are tabulated and rounded to the closest score between 1 and 5. The final scores are then used to build the 5x5 table that constitutes the NCCN Evidence Block™ for the intervention.
Each column in the NCCN Evidence Block™ [the "X" axis] corresponds to an outcome characteristic. From left to right, the outcome characteristics are efficacy (E), safety (S), quality and quantity of evidence (Q), consistency of data (C), and affordability (A).
The blocks within each column [the "Y" axis] are shaded in from bottom to top representing the corresponding score for each measure, "1" to "5".
Q. How do you compare NCCN Evidence Blocks™?
When the NCCN Evidence Blocks™ are placed within the NCCN Guidelines algorithms, a user can quickly scan a group of potentially appropriate interventions and make treatment recommendations based on what is most important to the patient.
Q. How does NCCN know what each therapy will cost?
The affordability measurement is not a hard cost to each patient; it represents an estimate of overall total cost of a therapy, including but not limited to drug acquisition, administration, in-patient vs. out-patient care, supportive care, infusions, toxicity monitoring, antiemetics and growth factors, and potential for hospitalization. The affordability measurement does not include indirect costs, such as transportation or time lost from work; nor does it attempt to assess direct cost to patients, as these costs vary widely based on individual circumstances. If affordability is of concern to an individual, a low score in the "A" column should be considered a catalyst for further discussion and investigation into the direct cost of a regimen for the patient.
Q. How can I request a change to the NCCN Guidelines with NCCN Evidence Blocks™?
NCCN Guidelines users can submit data to accompany a request for change or update to the NCCN Guidelines at any time. Learn more about submission requests.
In cancer care, the most important value perspective is that of the individual patient. NCCN Evidence Blocks™ educate providers and patients about the efficacy, safety, and affordability of systemic therapy. NCCN Evidence Blocks™ are a starting point for shared decision-making based on a common vocabulary of choices and values. The NCCN Evidence Blocks™ are published in a new version of the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) and are intended as a visual representation of five key value measures that provide important information about specific NCCN Guidelines® recommendations: efficacy, safety, quality and quantity of evidence, consistency of evidence, and affordability. Adding affordability to the existing National Comprehensive Cancer Network® (NCCN®) criteria for evaluating treatment options, empowers patients to identify, alongside their physician, optimal treatment based on clinical and economic considerations that are of most value to them. NCCN Guidelines with NCCN Evidence Blocks™ are an additional NCCN resource—separate from the NCCN Guidelines— that are currently available free of charge on NCCN.org.
For more information, visit NCCN.org/EvidenceBlocks.
NCCN Evidence Blocks™ are available for the following:
-
Acute Lymphoblastic Leukemia Version 2.2025
-
Acute Myeloid Leukemia Version 2.2025
-
Ampullary Adenocarcinoma Version 2.2025
-
Anal Carcinoma Version 4.2025
-
Basal Cell Skin Cancer Version 2.2025
-
B-Cell Lymphomas Version 2.2025
-
Biliary Tract Cancers Version 2.2025
-
Bladder Cancer Version 1.2025
-
Bone Cancer Version 2.2025
-
Breast Cancer Version 4.2025
-
Breast Cancer Risk Reduction Version 2.2025
-
Castleman Disease Version 2.2025
-
Central Nervous System Cancers Version 5.2024
-
Cervical Cancer Version 4.2025
-
Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma Version 3.2025
-
Chronic Myeloid Leukemia Version 3.2025
-
Colon Cancer Version 4.2025
-
Dermatofibrosarcoma Protuberans Version 1.2025
-
Esophageal and Esophagogastric Junction Cancers Version 3.2025
-
Gastric Cancer Version 2.2025
-
Gastrointestinal Stromal Tumors Version 1.2025
-
Gestational Trophoblastic Neoplasia Version 3.2025
-
Hairy Cell Leukemia Version 1.2025
-
Head and Neck Cancers Version 4.2025
-
Hepatocellular Carcinoma Version 1.2025
-
Histiocytic Neoplasms Version 1.2025
-
Hodgkin Lymphoma Version 2.2025
-
Kaposi Sarcoma Version 2.2025
-
Kidney Cancer Version 3.2025
-
Melanoma: Cutaneous Version 2.2025
-
Melanoma: Uveal Version 1.2025
-
Merkel Cell Carcinoma Version 2.2025
-
Mesothelioma: Pleural Version 2.2025
-
Multiple Myeloma Version 1.2026
-
Myelodysplastic Syndromes Version 2.2025
-
Myeloid/Lymphoid Neoplasms with Eosinophilia and Tyrosine Kinase Gene Fusions Version 2.2025
-
Myeloproliferative Neoplasms Version 2.2025
-
Neuroendocrine and Adrenal Tumors Version 2.2025
-
Non-Small Cell Lung Cancer Version 6.2025
-
Occult Primary Version 2.2025
-
Ovarian Cancer/Fallopian Tube Cancer/Primary Peritoneal Cancer Version 2.2025
-
Pancreatic Adenocarcinoma Version 2.2025
-
Pediatric Acute Lymphoblastic Leukemia Version 3.2025
-
Pediatric Aggressive Mature B-Cell Lymphomas Version 2.2025
-
Pediatric Central Nervous System Cancers Version 2.2025
-
Pediatric Hodgkin Lymphoma Version 2.2025
-
Penile Cancer Version 2.2025
-
Primary Cutaneous Lymphomas Version 3.2025
-
Prostate Cancer Version 2.2025
-
Rectal Cancer Version 2.2025
-
Small Bowel Adenocarcinoma Version 3.2025
-
Small Cell Lung Cancer Version 4.2025
-
Soft Tissue Sarcoma Version 1.2025
-
Squamous Cell Skin Cancer Version 2.2025
-
Systemic Light Chain Amyloidosis Version 1.2026
-
Systemic Mastocytosis Version 1.2025
-
T-Cell Lymphomas Version 2.2025
-
Testicular Cancer Version 2.2025
-
Thymomas and Thymic Carcinomas Version 2.2025
-
Thyroid Carcinoma Version 1.2025
-
Uterine Neoplasms Version 3.2025
-
Vaginal Cancer Version 5.2025
-
Vulvar Cancer Version 1.2025
-
Waldenström Macroglobulinemia/Lymphoplasmacytic Lymphoma Version 1.2026
